Understanding Ehlers-Danlos Syndrome (EDS)
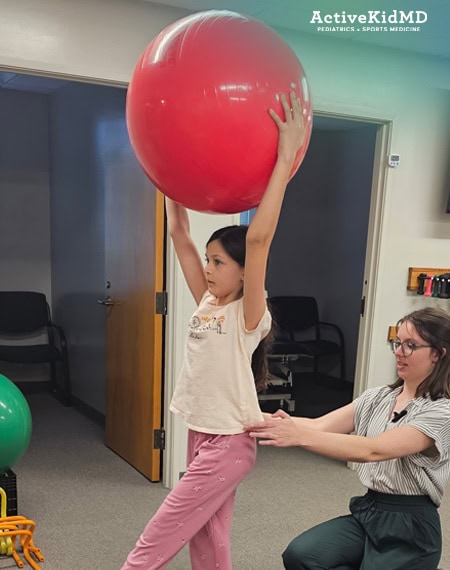
A collaboration between ActiveKidMD and Progressive Physical Therapy and Rehabilitation
May is Ehlers-Danlos Syndrome (EDS) and Hypermobility Spectrum Disorder (HSD) Awareness Month—a time to bring visibility to a condition that often goes unrecognized.

EDS refers to a group of hereditary connective tissue disorders that affect the structure and function of collagen in the body. This can lead to a wide range of symptoms, including joint hypermobility, subluxations/dislocations, frequent injuries, skin fragility, and systemic issues such as fatigue, gastrointestinal disturbances, and cardiovascular involvement.
The most common subtype, hypermobile EDS (hEDS), is often underdiagnosed or misdiagnosed. While not all people with joint hypermobility have EDS, nearly all individuals with hEDS experience some degree of joint hypermobility. According to estimates, hEDS may affect anywhere from 1 in 500 to 1 in 5,000 individuals, though the true prevalence is likely higher due to underdiagnosis (EDS Clinic).
Athletes in sports that emphasize flexibility and range of motion—such as gymnastics, dance, figure skating, and acrobatics—often exhibit higher rates of joint hypermobility. A study found that volleyball players had the highest rate of hypermobility, with 37.5% of participants showing advanced signs (ResearchGate).
A Pediatric Sports Medicine Perspective: Recognizing Patterns Early
Dr. Chris Koutures is a pediatric sports medicine physician at ActiveKidMD. He has an extensive background working with dancers, gymnasts, and volleyball athletes and notes that he often works backwards from symptoms to diagnosis.

Common findings in young athletes include:
- Joints that pop or dislocate
- Recurrent sprains or strains
- Excessive flexibility or hypermobility
- Fatigue, GI issues, thin skin
- Chest wall abnormalities (pectus) and scoliosis
(Pectus refers to structural deformities of the chest wall, such as pectus excavatum where the breastbone sinks inward, or pectus carinatum where it protrudes outward.)
Dr. Koutures emphasizes that identification often comes through observation—not just in clinical settings, but from coaches, instructors, and family members who notice something seems “off.” He’s seen increasing awareness in the community, especially among volleyball athletes with tall, slender frames.
“We see the beauty and grace of these athletes with their bendy bodies, but sometimes, that same flexibility can be a clue to something more complex going on beneath the surface.”
Once EDS is suspected, it opens the door to a broader, lifelong care journey. Dr. Koutures collaborates with a wide range of specialists including cardiologists, rheumatologists, and physical therapists to address the multi-system nature of EDS.
“This is not just about managing joints. It’s about managing a complex condition that can affect every part of the body. Coordinated care is essential.”
A Physical Therapy Perspective: Stabilizing and Supporting the Journey
At Progressive Physical Therapy and Rehabilitation, treatment of EDS and joint hypermobility begins with education and stabilization with progression into building strength, stamina, and postural control. Our approach is grounded in the Muldowney Protocol, a structured and research-based method tailored for hypermobility disorders. But just as importantly, it is informed by years of clinical experience working with EDS patients. No two individuals present the same way—so each receives a fully individualized care plan.
We also believe our patients. Many individuals with EDS have had their symptoms dismissed or misunderstood by medical professionals. When they say something feels off, we listen and adjust accordingly.
Ann Ludolph, MPT, OCS, at the Irvine Clinic of Progressive Physical Therapy and Rehab has years of experience helping patients with hEDS manage their symptoms through highly individualized, day-to-day adaptive care and progresses into building strength, stamina, and postural control.
“Our goal is to help stabilize what the body can’t. We retrain the nervous system, build strength, and give people the tools to move with confidence.”
“This is very much a collaborative approach,” she said. “What a cardiologist recommends might change how we structure a session. Likewise, if something isn’t working in therapy, the rest of the team needs to know. EDS is unpredictable—anything can flare. We adjust daily to help patients stay as stable as possible.”
Therapy goals typically focus on:
- Improving muscular strength and joint stability
- Increasing stamina and tolerance for activity
- Enhancing posture and motor control to prevent injuries
- Supporting the nervous system through pacing and education
Awareness Leads to Better Outcomes
EDS is one of many challenging conditions that often isn’t recognized right away—and too often, patients are left feeling unheard. That’s why finding a healthcare provider who truly listens, believes you, and works with you is so essential. Early recognition of EDS and hypermobility disorders can change the trajectory of a person’s health journey. Left undiagnosed, symptoms often escalate and interfere with daily function. However, with the right team, proactive care, and ongoing support, individuals with EDS can live active, fulfilling lives.
May is about awareness, education, and advocacy—so we can better support those living with EDS and empower communities to recognize the signs sooner and hopefully encourage them to seek the care that will improve their quality of life.


